Since its foundation in 1939, Frontier Nursing University (FNU) has adopted a mission of reaching rural, diverse and underserved populations. This mission is still being lived out today, where more than 80 FNU alumni are answering the call in Alaska. In the coming months, we will be highlighting several of these alumni who serve in our country’s most remote and unforgiving state.
 Karolina Priebe, DNP, ANP, FNP, Class 17 is the final alumna featured in our Alaska Spotlight series. She is a family nurse practitioner at Solstice Medicine and Wellness in Fairbanks.
Karolina Priebe, DNP, ANP, FNP, Class 17 is the final alumna featured in our Alaska Spotlight series. She is a family nurse practitioner at Solstice Medicine and Wellness in Fairbanks.
Fairbanks represents the last chance for medical care for many Alaskans living in the extreme northeast regions of the state.
“We are isolated from other areas of Alaska,” said Karolina. “We are really the northernmost city in northeast Alaska in terms of access to healthcare. We cover thousands of miles of the area.”
Born and raised in Poland, Karolina’s family moved to Chicago when she was 16. She eventually became a U.S. citizen and served as a medic in the military where she met her husband. His last station before retiring was Fairbanks in 2015. They fell in love with the community and continue to make their home there.
At Solstice Medicine and Wellness clinic, Karolina is the only primary care provider doing family practice daily. She is joined by an internal medicine physician and a physician’s assistant. Many of the patients they treat come from very remote locations and only visit the city once or twice a year.
“The bush people of Alaska have no roads,” Karolina said of the population made famous by the ‘Alaskan Bush People’ television series. “In summer they get to us via boat or four wheeler, and in the wintertime many travel by snow machine until they either reach a road system or a small airport. They come to town once every six months or once a year. We address as much as we can in one visit.”
That means a lot of acute care and little time left over for addressing lifestyle, education and preventative medicine, resulting in a gap that Karolina is trying to fill.
Noting a significant issue with obesity in her patient population, Karolina launched an obesity program in August 2018. She devotes approximately half her time providing primary care and the other half on the 60-80 people in the obesity program.
“Nobody is doing obesity management. In primary care, there’s no time to address that,” Karolina said. “Weight management is built into my work schedule for patients interested in medical weight loss. I’m treating chronic conditions such as diabetes and high blood pressure along with obesity at the same time. It saves the patient time and money.”
Patients in the program begin by keeping a food journal for a month. Karolina then reviews it and helps them find healthier alternatives to the foods they enjoy. Access to fresh and affordable healthy food is a significant hurdle for many in the community.
“There are many components to the obesity problem,” Karolina said. “A lot of my patients don’t have access to proper food. Fresh produce is very expensive here, especially in winter. Our food bank is a great resource but it mainly has packaged foods. A lot of people can’t afford the fresher, healthier foods.”
Affordability is also an issue when it comes to medical bills and, as a result, many are reluctant to seek the care they need. To help address this issue, Karolina serves on the board of KarmaCare, a local nonprofit that offers people assistance with their bills. Patients who qualify for the program are asked to volunteer in their community. In exchange for their service, KarmaCare will pay up to $4,000 per year toward their medical bills. “That’s the community we have,” Karolina said. “There is a unity of the community in Fairbanks and that’s why we stayed here.”
Another challenge facing the Fairbanks community is the limited amount of specialized care, so Karolina and her team arrange appointments with specialty care providers in Anchorage or Seattle. “Thankfully there’s a good working relationship between us and Anchorage and Seattle,” Karolina said. “They are good about working our referrals in. We have to sit on the phone for many hours to figure out where to send these patients.”
Karolina credits Frontier Nursing University with helping to prepare her to be innovative and community-driven in her work. “Frontier was all about going where there’s a need and making an impact,” Karolina said. “Every day I’m trying to see how I can help my patients, what’s needed, and how I can make an impact. I’m still trying to figure out how we can make medical care better here.
“Frontier is so focused on meeting patients where they are and making improvements in the community,” Karolina continued. “It prepared me to open my eyes to look at bigger issues, to look at what needs need to be addressed in the community to benefit not only the patients but their families as well.”
Thank you to Karolina, Kristina Amundson, David Moore and Holly Fisk who along with many other FNU alumni are answering the call to serve the underserved in Alaska.




 For the Fall 2019 term, Frontier Nursing University (FNU)’s featured preceptor is Ramona Scott, DNP, WHNP.
For the Fall 2019 term, Frontier Nursing University (FNU)’s featured preceptor is Ramona Scott, DNP, WHNP.  On November 21, 2019, healthcare providers and organizations across the country came together to celebrate National Rural Health Day (NRHD). Organized by the
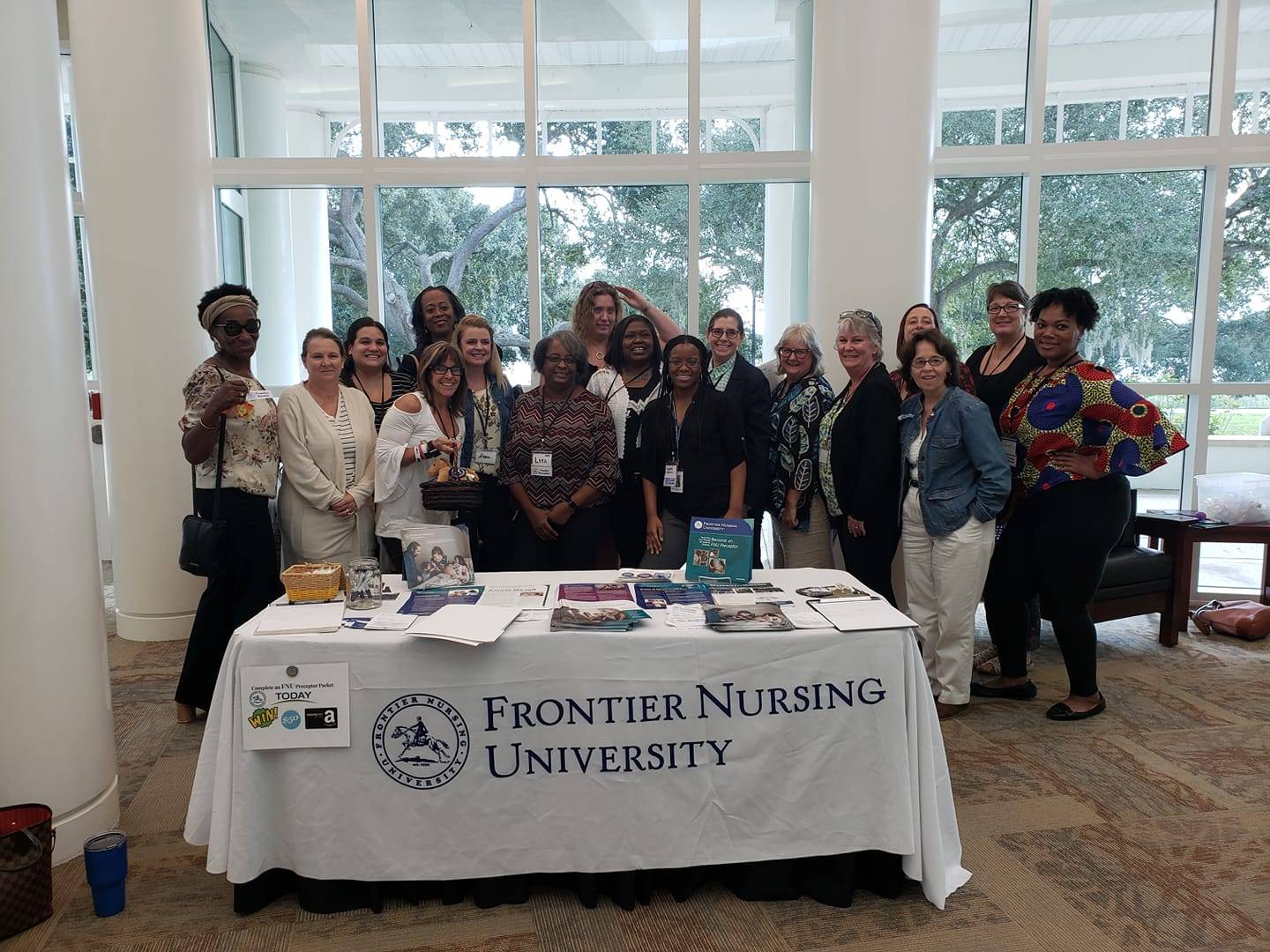
On November 21, 2019, healthcare providers and organizations across the country came together to celebrate National Rural Health Day (NRHD). Organized by the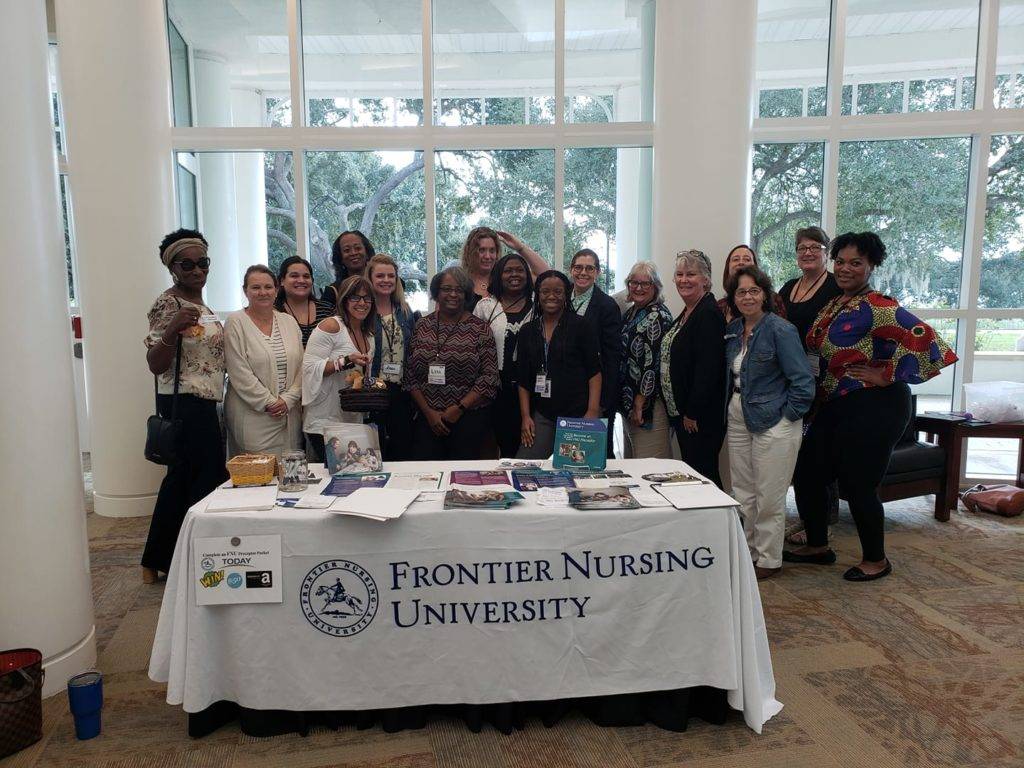 Representatives of Frontier Nursing University (FNU) recently attended the 2019 Florida State Affiliate
Representatives of Frontier Nursing University (FNU) recently attended the 2019 Florida State Affiliate 





 Since its foundation in 1939, Frontier Nursing University (FNU) has adopted a
Since its foundation in 1939, Frontier Nursing University (FNU) has adopted a  Frontier Nursing University (FNU) celebrated National Nurse Practitioner (NP) Week by hosting a
Frontier Nursing University (FNU) celebrated National Nurse Practitioner (NP) Week by hosting a Dr. Arterberry was taught the importance of reflection by her mother at a very young age, and she has certainly seen it ring true in her work in health care. In this session, Dr. Arterberry tells us that reflective practice is the foundation of professional development. It makes meaning from experience and transforms insights into practical strategies for personal growth and organizational impact. She emphasized that reflective practice is an active endeavor, not simply thinking about the past. Effective reflection allows leaders to challenge assumptions, review current practices, recognize harmful behaviors, and develop new ways of working. She gives us practical ways to implement critical reflection in our own lives, starting with structured journaling and through dialogue in a group setting.
Dr. Arterberry was taught the importance of reflection by her mother at a very young age, and she has certainly seen it ring true in her work in health care. In this session, Dr. Arterberry tells us that reflective practice is the foundation of professional development. It makes meaning from experience and transforms insights into practical strategies for personal growth and organizational impact. She emphasized that reflective practice is an active endeavor, not simply thinking about the past. Effective reflection allows leaders to challenge assumptions, review current practices, recognize harmful behaviors, and develop new ways of working. She gives us practical ways to implement critical reflection in our own lives, starting with structured journaling and through dialogue in a group setting. In this informative session on post-traumatic stress disorder, Dr. Calohan outlined the new DSM 5 diagnostic criteria implemented in 2014 that categorized PTSD separately from anxiety disorders. He reviewed the physical and psychological symptoms of different forms of PTSD. He told us about emerging neurobiological theories that are influencing new treatment methods, including targeting the endocannaboid system and GABA-B receptors associated with fear extinction. Dr. Calohan reviewed potential evidence-based treatment courses, going into the different options (or lack thereof) in the categories of anti-depressants, antipsychotics, mood stabilizers, benzodiazepines, and hypnotics. He also talked about the importance of sleep for PTSD patients and dove into evidence found in a recent study of the efficacy of Prazosin for trauma nightmares, giving advice on prescribing Prazosin. At the conclusion, Dr. Calohan provides a wealth of tools, external resources, and care models for PTSD patient care.
In this informative session on post-traumatic stress disorder, Dr. Calohan outlined the new DSM 5 diagnostic criteria implemented in 2014 that categorized PTSD separately from anxiety disorders. He reviewed the physical and psychological symptoms of different forms of PTSD. He told us about emerging neurobiological theories that are influencing new treatment methods, including targeting the endocannaboid system and GABA-B receptors associated with fear extinction. Dr. Calohan reviewed potential evidence-based treatment courses, going into the different options (or lack thereof) in the categories of anti-depressants, antipsychotics, mood stabilizers, benzodiazepines, and hypnotics. He also talked about the importance of sleep for PTSD patients and dove into evidence found in a recent study of the efficacy of Prazosin for trauma nightmares, giving advice on prescribing Prazosin. At the conclusion, Dr. Calohan provides a wealth of tools, external resources, and care models for PTSD patient care. Sepsis is deadly with delayed treatment and constitutes the number one hospital cost in America. In this session, Dr. Bray describes a project she instituted in response to concerning results on a survey of sepsis charts in the Tippah County Hospital Emergency Department. The project focused on four main areas: team engagement, patient engagement, sepsis screening, and the sepsis checklist. Dr. Bray reviewed the one-hour bundle for sepsis best practice that was implemented in the project. She discussed the adjustments they made as the project went on to continue to improve sepsis patient care, including simplifying tools, nurse initiated orders, and more effective interventions. The project results exceeded goals in each of the four categories, and Dr. Bray is now working on expanding the project to the Tippah County EMTs.
Sepsis is deadly with delayed treatment and constitutes the number one hospital cost in America. In this session, Dr. Bray describes a project she instituted in response to concerning results on a survey of sepsis charts in the Tippah County Hospital Emergency Department. The project focused on four main areas: team engagement, patient engagement, sepsis screening, and the sepsis checklist. Dr. Bray reviewed the one-hour bundle for sepsis best practice that was implemented in the project. She discussed the adjustments they made as the project went on to continue to improve sepsis patient care, including simplifying tools, nurse initiated orders, and more effective interventions. The project results exceeded goals in each of the four categories, and Dr. Bray is now working on expanding the project to the Tippah County EMTs. In the final session of the week, FNU NP faculty shared with us how each are serving the rural, diverse and underserved in their own communities. Led by Associate Dean of Family Nursing Lisa Chappell, PhD, FNP-BC, the session kicked off with Nena Harris, PhD, FNP-BC, CNM, CNE who talked about integrating a comprehensive case management model of health care to homeless women and children in Charlotte, N.C. Nikita Duke, DNP, PMHNP-BC discussed the need for integrating behavioral access care into the urgent care environment in her Muscle Shoals, Ala. community. Diane John, PhD, APRN, FNP-BC, CNE told us about her work in Miramar, Fla., fostering relationships with community partners and community dwellers, and providing leadership opportunities for nurse practitioners.
In the final session of the week, FNU NP faculty shared with us how each are serving the rural, diverse and underserved in their own communities. Led by Associate Dean of Family Nursing Lisa Chappell, PhD, FNP-BC, the session kicked off with Nena Harris, PhD, FNP-BC, CNM, CNE who talked about integrating a comprehensive case management model of health care to homeless women and children in Charlotte, N.C. Nikita Duke, DNP, PMHNP-BC discussed the need for integrating behavioral access care into the urgent care environment in her Muscle Shoals, Ala. community. Diane John, PhD, APRN, FNP-BC, CNE told us about her work in Miramar, Fla., fostering relationships with community partners and community dwellers, and providing leadership opportunities for nurse practitioners. Frontier Nursing University (FNU) is pleased to announce the 2019 Summer Term Circle of Caring Award Winners: staff member Jamie Wheeler and faculty member Lisa Chappell.
Frontier Nursing University (FNU) is pleased to announce the 2019 Summer Term Circle of Caring Award Winners: staff member Jamie Wheeler and faculty member Lisa Chappell. Jamie is one of two clinical advisors at FNU who support students with their clinical site and preceptor search. She meets one-on-one with students, leads clinical search webinars, and attends Frontier Bound orientation sessions to meet with new students.
Jamie is one of two clinical advisors at FNU who support students with their clinical site and preceptor search. She meets one-on-one with students, leads clinical search webinars, and attends Frontier Bound orientation sessions to meet with new students. Lisa is an associate professor and the associate dean of family nursing at FNU. She works with fellow faculty and staff to problem-solve and offer support.
Lisa is an associate professor and the associate dean of family nursing at FNU. She works with fellow faculty and staff to problem-solve and offer support.


















 Carrie Belin is an experienced board-certified Family Nurse Practitioner and a graduate of the Johns Hopkins DNP program, Johns Hopkins Bloomberg School of Public Health, Georgetown University School of Nursing, and Johns Hopkins School of Nursing. She has also completed fellowships at Georgetown and the University of California Irvine.
Carrie Belin is an experienced board-certified Family Nurse Practitioner and a graduate of the Johns Hopkins DNP program, Johns Hopkins Bloomberg School of Public Health, Georgetown University School of Nursing, and Johns Hopkins School of Nursing. She has also completed fellowships at Georgetown and the University of California Irvine. Angie has been a full-scope midwife since 2009. She has experience in various birth settings including home, hospital, and birth centers. She is committed to integrating the midwifery model of care in the US. She completed her master’s degree in nurse-midwifery at Frontier Nursing University (FNU) and her Doctorate at Johns Hopkins University. She currently serves as the midwifery clinical faculty at FNU. Angie is motivated by the desire to improve the quality of healthcare and has led quality improvement projects on skin-to-skin implementation, labor induction, and improving transfer of care practices between hospital and community midwives. In 2017, she created a short film on skin-to-skin called
Angie has been a full-scope midwife since 2009. She has experience in various birth settings including home, hospital, and birth centers. She is committed to integrating the midwifery model of care in the US. She completed her master’s degree in nurse-midwifery at Frontier Nursing University (FNU) and her Doctorate at Johns Hopkins University. She currently serves as the midwifery clinical faculty at FNU. Angie is motivated by the desire to improve the quality of healthcare and has led quality improvement projects on skin-to-skin implementation, labor induction, and improving transfer of care practices between hospital and community midwives. In 2017, she created a short film on skin-to-skin called 










 Justin C. Daily, BSN, RN, has ten years of experience in nursing. At the start of his nursing career, Justin worked as a floor nurse on the oncology floor at St. Francis. He then spent two years as the Director of Nursing in a small rural Kansas hospital before returning to St. Francis and the oncology unit. He has been in his current position as the Chemo Nurse Educator for the past four years. He earned an Associate in Nurse from Hutchinson Community College and a Bachelor of Science in Nursing from Bethel College.
Justin C. Daily, BSN, RN, has ten years of experience in nursing. At the start of his nursing career, Justin worked as a floor nurse on the oncology floor at St. Francis. He then spent two years as the Director of Nursing in a small rural Kansas hospital before returning to St. Francis and the oncology unit. He has been in his current position as the Chemo Nurse Educator for the past four years. He earned an Associate in Nurse from Hutchinson Community College and a Bachelor of Science in Nursing from Bethel College. Brandy Jackson serves as the Director of Undergraduate Nursing Programs and Assistant Educator at Wichita State University and Co-Director of Access in Nursing. Brandy is a seasoned educator with over 15 years of experience. Before entering academia, Brandy served in Hospital-based leadership and Critical Care Staff nurse roles. Brandy is passionate about equity in nursing education with a focus on individuals with disabilities. Her current research interests include accommodations of nursing students with disabilities in clinical learning environments and breaking down barriers for historically unrepresented individuals to enter the nursing profession. Brandy is also actively engaged in Interprofessional Education development, creating IPE opportunities for faculty and students at Wichita State. Brandy is an active member of Wichita Women for Good and Soroptimist, with the goal to empower women and girls. Brandy is a TeamSTEPPS master trainer. She received the DASIY Award for Extraordinary Nursing Faculty in 2019 at Wichita State University.
Brandy Jackson serves as the Director of Undergraduate Nursing Programs and Assistant Educator at Wichita State University and Co-Director of Access in Nursing. Brandy is a seasoned educator with over 15 years of experience. Before entering academia, Brandy served in Hospital-based leadership and Critical Care Staff nurse roles. Brandy is passionate about equity in nursing education with a focus on individuals with disabilities. Her current research interests include accommodations of nursing students with disabilities in clinical learning environments and breaking down barriers for historically unrepresented individuals to enter the nursing profession. Brandy is also actively engaged in Interprofessional Education development, creating IPE opportunities for faculty and students at Wichita State. Brandy is an active member of Wichita Women for Good and Soroptimist, with the goal to empower women and girls. Brandy is a TeamSTEPPS master trainer. She received the DASIY Award for Extraordinary Nursing Faculty in 2019 at Wichita State University.  Dr. Sabrina Ali Jamal-Eddine is an Arab-disabled queer woman of color with a PhD in Nursing and an interdisciplinary certificate in Disability Ethics from the University of Illinois Chicago (UIC). Dr. Jamal-Eddine’s doctoral research explored spoken word poetry as a form of critical narrative pedagogy to educate nursing students about disability, ableism, and disability justice. Dr. Jamal-Eddine now serves as a Postdoctoral Research Associate in UIC’s Department of Disability and Human Development and serves on the Board of Directors of the National Organization of Nurses with Disabilities (NOND). During her doctoral program, Sabrina served as a Summer Fellow at a residential National Endowment of the Humanities (NEH) Summer Institute at Arizona State University (2023), a summer fellow at Andrew W. Mellon’s National Humanities Without Walls program at University of Michigan (2022), a Summer Research Fellow at UC Berkeley’s Othering & Belonging Institute (2021), and an Illinois Leadership Education in Neurodevelopmental and related Disabilities (LEND) trainee (2019-2020).
Dr. Sabrina Ali Jamal-Eddine is an Arab-disabled queer woman of color with a PhD in Nursing and an interdisciplinary certificate in Disability Ethics from the University of Illinois Chicago (UIC). Dr. Jamal-Eddine’s doctoral research explored spoken word poetry as a form of critical narrative pedagogy to educate nursing students about disability, ableism, and disability justice. Dr. Jamal-Eddine now serves as a Postdoctoral Research Associate in UIC’s Department of Disability and Human Development and serves on the Board of Directors of the National Organization of Nurses with Disabilities (NOND). During her doctoral program, Sabrina served as a Summer Fellow at a residential National Endowment of the Humanities (NEH) Summer Institute at Arizona State University (2023), a summer fellow at Andrew W. Mellon’s National Humanities Without Walls program at University of Michigan (2022), a Summer Research Fellow at UC Berkeley’s Othering & Belonging Institute (2021), and an Illinois Leadership Education in Neurodevelopmental and related Disabilities (LEND) trainee (2019-2020). Vanessa Cameron works for Vanderbilt University Medical Center in Nursing Education & Professional Development. She is also attending George Washington University and progressing towards a PhD in Nursing with an emphasis on ableism in nursing. After becoming disabled in April 2021, Vanessa’s worldview and perspective changed, and a recognition of the ableism present within healthcare and within the culture of nursing was apparent. She has been working since that time to provide educational foundations for nurses about disability and ableism, provide support for fellow disabled nursing colleagues, and advocate for the disabled community within healthcare settings to reduce disparities.
Vanessa Cameron works for Vanderbilt University Medical Center in Nursing Education & Professional Development. She is also attending George Washington University and progressing towards a PhD in Nursing with an emphasis on ableism in nursing. After becoming disabled in April 2021, Vanessa’s worldview and perspective changed, and a recognition of the ableism present within healthcare and within the culture of nursing was apparent. She has been working since that time to provide educational foundations for nurses about disability and ableism, provide support for fellow disabled nursing colleagues, and advocate for the disabled community within healthcare settings to reduce disparities. Dr. Lucinda Canty is a certified nurse-midwife, Associate Professor of Nursing, and Director of the Seedworks Health Equity in Nursing Program at the University of Massachusetts Amherst. She earned a bachelor’s degree in nursing from Columbia University, a master’s degree from Yale University, specializing in nurse-midwifery, and a PhD from the University of Connecticut. Dr. Canty has provided reproductive health care for over 29 years. Her research interests include the prevention of maternal mortality and severe maternal morbidity, reducing racial and ethnic health disparities in reproductive health, promoting diversity in nursing, and eliminating racism in nursing and midwifery.
Dr. Lucinda Canty is a certified nurse-midwife, Associate Professor of Nursing, and Director of the Seedworks Health Equity in Nursing Program at the University of Massachusetts Amherst. She earned a bachelor’s degree in nursing from Columbia University, a master’s degree from Yale University, specializing in nurse-midwifery, and a PhD from the University of Connecticut. Dr. Canty has provided reproductive health care for over 29 years. Her research interests include the prevention of maternal mortality and severe maternal morbidity, reducing racial and ethnic health disparities in reproductive health, promoting diversity in nursing, and eliminating racism in nursing and midwifery. Dr. Lisa Meeks is a distinguished scholar and leader whose unwavering commitment to inclusivity and excellence has significantly influenced the landscape of health professions education and accessibility. She is the founder and executive director of the DocsWithDisabilities Initiative and holds appointments as an Associate Professor in the Departments of Learning Health Sciences and Family Medicine at the University of Michigan.
Dr. Lisa Meeks is a distinguished scholar and leader whose unwavering commitment to inclusivity and excellence has significantly influenced the landscape of health professions education and accessibility. She is the founder and executive director of the DocsWithDisabilities Initiative and holds appointments as an Associate Professor in the Departments of Learning Health Sciences and Family Medicine at the University of Michigan. Dr. Nikia Grayson, DNP, MSN, MPH, MA, CNM, FNP-C, FACNM (she/her) is a trailblazing force in reproductive justice, blending her expertise as a public health activist, anthropologist, and family nurse-midwife to champion the rights and health of underserved communities. Graduating with distinction from Howard University, Nikia holds a bachelor’s degree in communications and a master’s degree in public health. Her academic journey also led her to the University of Memphis, where she earned a master’s in medical anthropology, and the University of Tennessee, where she achieved both a master’s in nursing and a doctorate in nursing practice. Complementing her extensive education, she completed a post-master’s certificate in midwifery at Frontier Nursing University.
Dr. Nikia Grayson, DNP, MSN, MPH, MA, CNM, FNP-C, FACNM (she/her) is a trailblazing force in reproductive justice, blending her expertise as a public health activist, anthropologist, and family nurse-midwife to champion the rights and health of underserved communities. Graduating with distinction from Howard University, Nikia holds a bachelor’s degree in communications and a master’s degree in public health. Her academic journey also led her to the University of Memphis, where she earned a master’s in medical anthropology, and the University of Tennessee, where she achieved both a master’s in nursing and a doctorate in nursing practice. Complementing her extensive education, she completed a post-master’s certificate in midwifery at Frontier Nursing University.









 Dr. Tia Brown McNair is the Vice President in the Office of Diversity, Equity, and Student Success and Executive Director for the Truth, Racial Healing, and Transformation (TRHT) Campus Centers at the American Association of Colleges and Universities (AAC&U) in Washington, DC. She oversees both funded projects and AAC&U’s continuing programs on equity, inclusive excellence, high-impact practices, and student success. McNair directs AAC&U’s Summer Institutes on High-Impact Practices and Student Success, and TRHT Campus Centers and serves as the project director for several AAC&U initiatives, including the development of a TRHT-focused campus climate toolkit. She is the lead author of From Equity Talk to Equity Walk: Expanding Practitioner Knowledge for Racial Justice in Higher Education (January 2020) and Becoming a Student-Ready College: A New Culture of Leadership for Student Success (July 2016 and August 2022 Second edition).
Dr. Tia Brown McNair is the Vice President in the Office of Diversity, Equity, and Student Success and Executive Director for the Truth, Racial Healing, and Transformation (TRHT) Campus Centers at the American Association of Colleges and Universities (AAC&U) in Washington, DC. She oversees both funded projects and AAC&U’s continuing programs on equity, inclusive excellence, high-impact practices, and student success. McNair directs AAC&U’s Summer Institutes on High-Impact Practices and Student Success, and TRHT Campus Centers and serves as the project director for several AAC&U initiatives, including the development of a TRHT-focused campus climate toolkit. She is the lead author of From Equity Talk to Equity Walk: Expanding Practitioner Knowledge for Racial Justice in Higher Education (January 2020) and Becoming a Student-Ready College: A New Culture of Leadership for Student Success (July 2016 and August 2022 Second edition).