The Frontier community is proud to have students and alumni serving on the frontlines of the COVID-19 pandemic. Throughout the next few weeks, we are committed to sharing their stories in order to provide insight, hope and encouragement. Thank you to all the health care workers who are risking their own well-being daily to serve our nation. Click here to read more stories of courage and dedication.
The COVID-19 Pandemic has forced healthcare providers to be flexible and innovative in how they provide care. From greater access to telehealth appointments to drive-up COVID-19 testing, social distancing and limiting exposure has been the driving force for change.
Ginny Bowers, CNM, IBCLC, RLC, Class 82, shared her own innovation on social media on March 18. The post, accompanied by a photo, simply read: “Mobile midwifery! Taking care of my pregnant mamas in their cars in order to help out our community.”
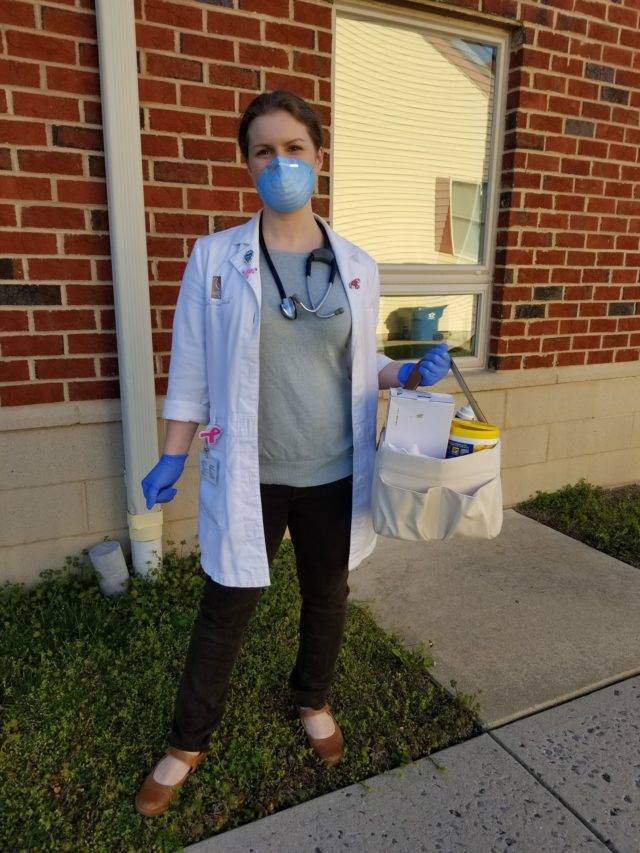 As the Head Midwife at Chesapeake Women’s Health in Easton, Maryland, Bowers recognized the need to reduce risks of exposure to her pregnant patients. Having them come into the office for appointments added risks that could be avoided by offering a drive-up option.
As the Head Midwife at Chesapeake Women’s Health in Easton, Maryland, Bowers recognized the need to reduce risks of exposure to her pregnant patients. Having them come into the office for appointments added risks that could be avoided by offering a drive-up option.
“I reached this decision due to significant concerns with exposure of our pregnant patients to COVID-19,” Bowers explained. “Pregnant women carry a significantly higher risk of complications when exposed to respiratory viruses, and I wanted to help decrease that risk in any way possible. We are fortunate that our office provides multiple outside doors and we have a parking lot that wraps around to the side of the building. I have my pregnant patients drive to that side parking lot and they call the practice to inform us that they are here. I then go directly to their cars and function as both a medical assistant and provider. I obtain blood pressures, fetal heart tones, maternal heart rate and fundal heights without the patients leaving their cars.”
In addition, the door to the side parking lot is right next to a patient bathroom, allowing patients to obtain a self-collect swab or urine sample with limited exposure to others in the office. There is also a direct door to the lab and ultrasound locations, allowing patients easy access from their car without ever setting foot in the waiting room.
Bowers takes great precaution to protect the patient, including limiting the number of staff the patient comes in contact with.
“I elected to function as both the medical assistant and the provider so as to limit the patient’s exposure,” Bowers said. “I wear a surgical mask and gloves to provide further protection to them in case I eventually become an asymptomatic carrier. If we do have a patient presenting with any symptoms we also have the patient and myself wear full PPE.”
Originally from Richmond, Virginia, Bowers previously worked as a registered nurse in Richmond before moving to the Eastern Shore of Maryland in 2014. Her decision to become a nurse-midwife was driven by a desire to better serve patients and her own near-tragedy.
“I am a strong advocate for patient autonomy and patient-centered care,” she said. “As a registered nurse I had planned on specializing in either trauma or emergency medicine, but when I was pregnant with my first daughter my labor and delivery became unnecessarily complicated and grossly mismanaged. At the age of 25, I almost died and became a statistic reflective of our broken healthcare system. When seeking answers on ways to better advocate for my patients I discovered midwifery and it was the perfect fit. This was the way I would be able to help protect others from suffering the same complications and fate that I had.”
Fate led her to FNU, which she credits for helping prepare her for the innovative thinking needed in situations such as the pandemic.
“Frontier is a fabulous university and I truly believe this organization helped foster my ability to problem solve and seek out solutions,” Bowers said. “Midwives really have a way of thinking outside of the box.”
Chesapeake Women’s Health is a multidisciplinary practice where Bowers works alongside obstetricians. She works autonomously within the practice providing full-scope OB/GYN and lactation services and attending births at the local hospital.
“I am fortunate that I work in a practice that is both receptive and willing to accommodate my suggestions for improving patient care,” said Bowers, who works alongside four other nurse-midwives, including Becky Kroeger, CNM, a fellow FNU graduate (Class 106). “We have a fabulous office manager in Jessica Lewis and supervisor in Kristina Lynch who are also strong advocates for patient safety and evidence-based practice. I work alongside both physicians and midwives and have been especially proud especially of my midwife colleagues as together we have really raised the bar for patient safety. We have also initiated a thriving telemedicine practice and have arranged our hospital and office schedules in a way that will minimize staff mixing and exposures so we can better protect our providers who are critical to this rural area.”
The nurse-midwives have arranged their schedules so that one practices solo in the office while the other three manage hospital call. None of them are exposed to each other, thus decreasing the risk of having multiple providers out sick at the same time. Like healthcare providers across the country, Chesapeake Women’s Health has had to deal with a lack of available testing and PPE supplies.
That’s where out-of-the-box thinking by Bowers and her colleagues has led to the changes in work schedules and the mobile midwifery practice to reduce the risk for staff and patients alike. Patients were made aware of the curbside prenatal service by phone calls and social media posts.
“Patients are scared due to all of the unknowns,” Bowers said. “They have loved this service and have been extremely grateful for this option.”
Amidst the chaos, Bowers stands ready in the parking lot, taking care of her patients, one car at a time.
What is a Certified Nurse-Midwife (CNM)?
Certified Nurse-Midwives (CNMs) are educated in two disciplines: midwifery and nursing. They earn graduate degrees, complete a midwifery education program accredited by the Accreditation Commission for Midwifery Education (ACME), and pass a national certification examination administered by the American Midwifery Certification Board (AMCB) to receive the professional designation of CNM. Certified Midwives (CMs) are educated in the discipline of midwifery. They earn graduate degrees, meet health and science education requirements, complete a midwifery education program accredited by ACME, and pass the same national certification examination as CNMs to receive the professional designation of CM.




 Dr. Nikia Grayson, DNP, MSN, MPH, MA, CNM, FNP-C, FACNM (she/her) is a trailblazing force in reproductive justice, blending her expertise as a public health activist, anthropologist, and family nurse-midwife to champion the rights and health of underserved communities. Graduating with distinction from Howard University, Nikia holds a bachelor’s degree in communications and a master’s degree in public health. Her academic journey also led her to the University of Memphis, where she earned a master’s in medical anthropology, and the University of Tennessee, where she achieved both a master’s in nursing and a doctorate in nursing practice. Complementing her extensive education, she completed a post-master’s certificate in midwifery at Frontier Nursing University.
Dr. Nikia Grayson, DNP, MSN, MPH, MA, CNM, FNP-C, FACNM (she/her) is a trailblazing force in reproductive justice, blending her expertise as a public health activist, anthropologist, and family nurse-midwife to champion the rights and health of underserved communities. Graduating with distinction from Howard University, Nikia holds a bachelor’s degree in communications and a master’s degree in public health. Her academic journey also led her to the University of Memphis, where she earned a master’s in medical anthropology, and the University of Tennessee, where she achieved both a master’s in nursing and a doctorate in nursing practice. Complementing her extensive education, she completed a post-master’s certificate in midwifery at Frontier Nursing University.









 Dr. Tia Brown McNair is the Vice President in the Office of Diversity, Equity, and Student Success and Executive Director for the Truth, Racial Healing, and Transformation (TRHT) Campus Centers at the American Association of Colleges and Universities (AAC&U) in Washington, DC. She oversees both funded projects and AAC&U’s continuing programs on equity, inclusive excellence, high-impact practices, and student success. McNair directs AAC&U’s Summer Institutes on High-Impact Practices and Student Success, and TRHT Campus Centers and serves as the project director for several AAC&U initiatives, including the development of a TRHT-focused campus climate toolkit. She is the lead author of From Equity Talk to Equity Walk: Expanding Practitioner Knowledge for Racial Justice in Higher Education (January 2020) and Becoming a Student-Ready College: A New Culture of Leadership for Student Success (July 2016 and August 2022 Second edition).
Dr. Tia Brown McNair is the Vice President in the Office of Diversity, Equity, and Student Success and Executive Director for the Truth, Racial Healing, and Transformation (TRHT) Campus Centers at the American Association of Colleges and Universities (AAC&U) in Washington, DC. She oversees both funded projects and AAC&U’s continuing programs on equity, inclusive excellence, high-impact practices, and student success. McNair directs AAC&U’s Summer Institutes on High-Impact Practices and Student Success, and TRHT Campus Centers and serves as the project director for several AAC&U initiatives, including the development of a TRHT-focused campus climate toolkit. She is the lead author of From Equity Talk to Equity Walk: Expanding Practitioner Knowledge for Racial Justice in Higher Education (January 2020) and Becoming a Student-Ready College: A New Culture of Leadership for Student Success (July 2016 and August 2022 Second edition).