Dr. Nagavalli Thiruvalluvan, DNP (Class 47), APN, NP-C, CRRN
Frontier Nursing University alumna Dr. Nagavalli Thiruvalluvan, DNP (Class 47), APN, NP-C, CRRN, migrated from India to the United States in 1995, along with her husband and 2-month-old baby. Since then, she has achieved a remarkable nursing career, including the completion of her Post-Master’s Doctor of Nursing Practice (DNP) from FNU in 2023.
Since 2020, Dr. Thiruvalluvan has owned and operated Adult & Geriatric Primary Care in Metuchen, NJ. The suburban borough, located outside of Staten Island, NY, features a diverse population of Caucasian, Asian, African American, and Hispanic residents. She has provided primary care for adult and geriatric patients in the community focusing on individualized care based on cultural values and beliefs.
Because the opening of her clinic coincided with the COVID-19 pandemic, Dr. Thiruvalluvan initially focused her efforts on going above and beyond in helping patients with COVID-19 testing and treating acute illnesses via telemedicine. She now cares for her patients by providing weight loss management, offering preventative care through education and counseling, and following evidence-based guidelines. She is also passionate about providing medical care to the geriatric population at the clinic, but also in their homes.
“My goal is to treat patients and address all their needs within the scope of my practice,” said Dr. Thiruvalluvan. “I genuinely see the reward of my work in patient statements and satisfaction.”
As an entrepreneur and nurse practitioner, Dr. Thiruvalluvan realized that she needed to expand her knowledge to the doctoral level and get involved with advocacy and policy making, as she encountered bias with insurance companies and physician colleagues who failed to acknowledge the full potential of the practitioner role.
Acting on advice from one of her colleagues, Dr. Thiruvalluvan began her DNP journey at FNU in June of 2022 while continuing to work in her primary care practice. She found the didactic courses to be very helpful as she prepared for her overall DNP project, including PC727: Ethics and Health Policy, where she learned how to identify health-related social issues in the community and dive into the problems.
“It provided me with the knowledge to approach policymakers to address these kinds of issues and fix them at the community level,” said Dr. Thiruvalluvan.
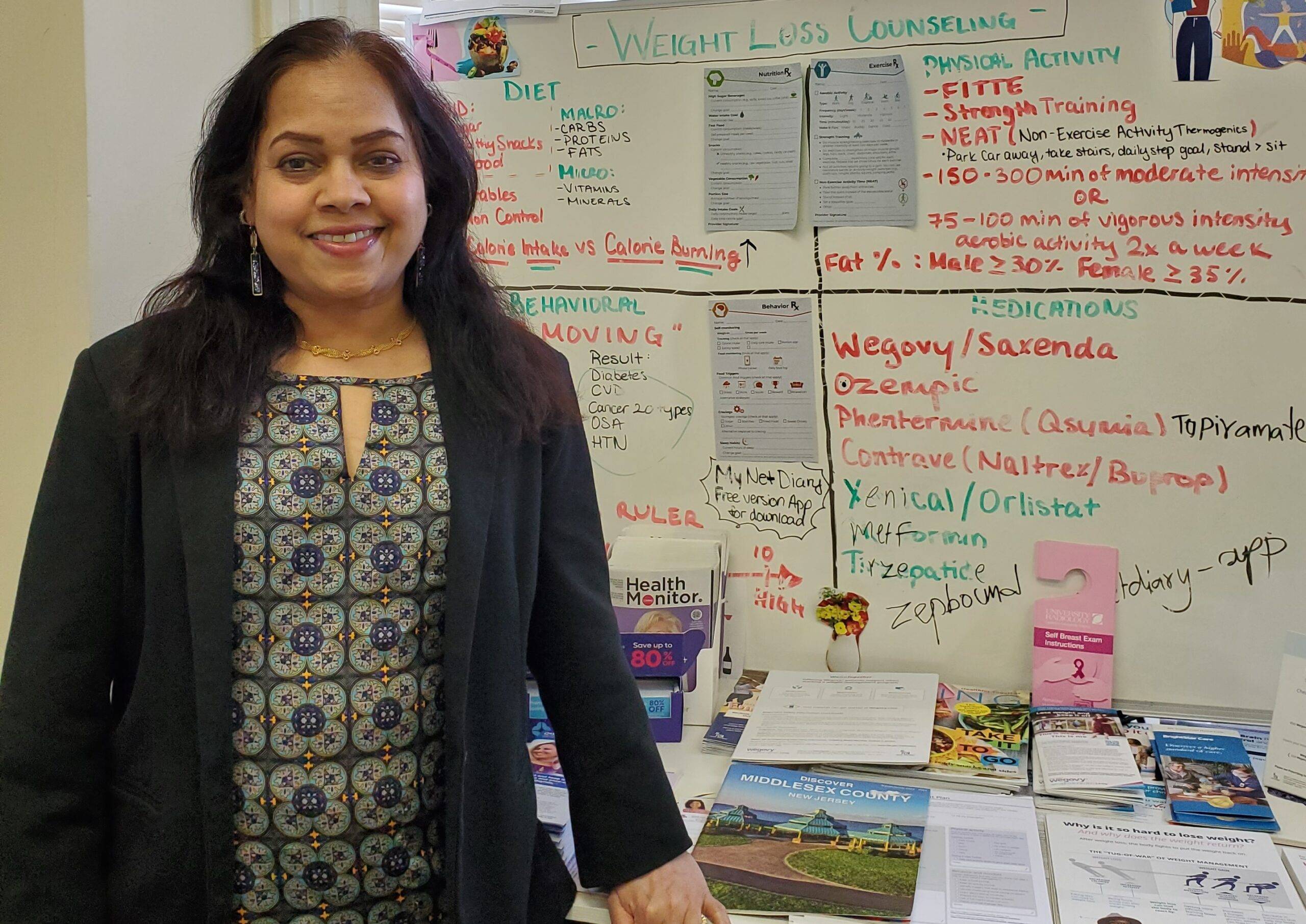
For her DNP project, Dr. Thiruvalluvan developed a weight management program for her primary care clinic, where 75% of her patients had a BMI of 27 or above. She set a goal that 90% of her patient population dealing with weight management issues would achieve their desired goal weight through comprehensive lifestyle modifications.
And then, the pounds started coming off!
With Dr. Thiruvalluvan’s renewed emphasis on preventative care and weight loss management, her patients were able to manage and control comorbidities as they started losing weight. Patients also experienced improved body image and many of them resolved other health conditions, with several medications being reduced or eliminated.
“The biggest reward was seeing evident patient outcomes due to treatment,” said Dr. Thiruvalluvan.
Prior to her DNP journey, Dr. Thiruvalluvan focused on equity when delivering patient care. However, she learned to acknowledge diversity and varied treatment options when delivering individualized care. Her quality improvement (QI) project was especially valuable in not only broadening her knowledge, but also in helping her address weight gain issues and their consequences on her patients at a deeper clinical level.
Dr. Thiruvalluvan identified her project focus while taking PC739: DNP Clinical Prep 101. In addition to supporting overall project preparation, the course also served as an essential starting point to navigating resources for her topic. She then progressed to the DNP planning section, requiring her to learn Google forms, patient data collection, and how to measure her progress through the course workbook and operation definitions.
About FNU DNP Projects
DNP projects are guided by the needs of the clinical site. Projects are small in scope and need to be appropriate for implementation within three months of the student and sponsor deciding on the clinical topic. Students complete planned improvements using the Institute for Healthcare Improvement “Model for Improvement” over an eight-week period. Examples include: improving compliance with childhood vaccination appointments, implementation of a palliative care shared decision making tool, initiating bedside huddles, or utilization of a toolkit related to a nationally endorsed quality measure.
“The operational definitions in the planning section of the course workbook were difficult to wrap my head around,” Dr. Thiruvalluvan reflected, “but they were very useful and tremendously helpful with patient data collection and generating my statistics.”
During project planning and implementation, Dr. Thiruvalluvan and her mentor met biweekly so she could provide updates regarding her progress and discuss the need for improvement and changes if needed.
Through her QI project experience, Dr. Thiruvalluvan was taught to provide the best care available for patients by analyzing evidence through data collection. By learning the importance of practicing scientific, evidence-based care, she was able to improve how she provides safe, effective, and quality care to her patients. The project also pushed her to better advocate for her patients.
“DNP-prepared nurses can improve healthcare outcomes in this country and lead to saving millions of dollars in healthcare costs,” she said.

DNP Program Overview
- Complete your coursework online.
- Complete 30 credit hours in 18 months.
- In collaboration with your clinical site, lead a rapid cycle quality improvement project (500 clinical hours).
- One three-day campus immersion experience (orientation before beginning the program).
- Small cohort of students.
“I recommend students pursue their DNP through FNU, as it teaches you how to think critically and address healthcare in a broader spectrum,” Dr. Thiruvalluvan continued. “By learning more about your key role as a healthcare provider, you will understand how you can be more influential to patients and the healthcare team.”
Dr. Thiruvalluvan truly enjoys her days working with patients in the clinic and seeing how their healthcare outcomes improve. Outside of work, she keeps herself updated with medical and political news, and likes cooking, shopping, and spending time with her 2-year old dog, Sony.
Learn more about advanced nursing degrees and specialties at Frontier Nursing University. Subscribe to our blog for the latest news and events at FNU and to get inspired with stories featuring our alumni, students, faculty, preceptors and staff!
















 Carrie Belin is an experienced board-certified Family Nurse Practitioner and a graduate of the Johns Hopkins DNP program, Johns Hopkins Bloomberg School of Public Health, Georgetown University School of Nursing, and Johns Hopkins School of Nursing. She has also completed fellowships at Georgetown and the University of California Irvine.
Carrie Belin is an experienced board-certified Family Nurse Practitioner and a graduate of the Johns Hopkins DNP program, Johns Hopkins Bloomberg School of Public Health, Georgetown University School of Nursing, and Johns Hopkins School of Nursing. She has also completed fellowships at Georgetown and the University of California Irvine.












 Angie has been a full-scope midwife since 2009. She has experience in various birth settings including home, hospital, and birth centers. She is committed to integrating the midwifery model of care in the US. She completed her master’s degree in nurse-midwifery at Frontier Nursing University (FNU) and her Doctorate at Johns Hopkins University. She currently serves as the midwifery clinical faculty at FNU. Angie is motivated by the desire to improve the quality of healthcare and has led quality improvement projects on skin-to-skin implementation, labor induction, and improving transfer of care practices between hospital and community midwives. In 2017, she created a short film on skin-to-skin called
Angie has been a full-scope midwife since 2009. She has experience in various birth settings including home, hospital, and birth centers. She is committed to integrating the midwifery model of care in the US. She completed her master’s degree in nurse-midwifery at Frontier Nursing University (FNU) and her Doctorate at Johns Hopkins University. She currently serves as the midwifery clinical faculty at FNU. Angie is motivated by the desire to improve the quality of healthcare and has led quality improvement projects on skin-to-skin implementation, labor induction, and improving transfer of care practices between hospital and community midwives. In 2017, she created a short film on skin-to-skin called 

 Justin C. Daily, BSN, RN, has ten years of experience in nursing. At the start of his nursing career, Justin worked as a floor nurse on the oncology floor at St. Francis. He then spent two years as the Director of Nursing in a small rural Kansas hospital before returning to St. Francis and the oncology unit. He has been in his current position as the Chemo Nurse Educator for the past four years. He earned an Associate in Nurse from Hutchinson Community College and a Bachelor of Science in Nursing from Bethel College.
Justin C. Daily, BSN, RN, has ten years of experience in nursing. At the start of his nursing career, Justin worked as a floor nurse on the oncology floor at St. Francis. He then spent two years as the Director of Nursing in a small rural Kansas hospital before returning to St. Francis and the oncology unit. He has been in his current position as the Chemo Nurse Educator for the past four years. He earned an Associate in Nurse from Hutchinson Community College and a Bachelor of Science in Nursing from Bethel College. Brandy Jackson serves as the Director of Undergraduate Nursing Programs and Assistant Educator at Wichita State University and Co-Director of Access in Nursing. Brandy is a seasoned educator with over 15 years of experience. Before entering academia, Brandy served in Hospital-based leadership and Critical Care Staff nurse roles. Brandy is passionate about equity in nursing education with a focus on individuals with disabilities. Her current research interests include accommodations of nursing students with disabilities in clinical learning environments and breaking down barriers for historically unrepresented individuals to enter the nursing profession. Brandy is also actively engaged in Interprofessional Education development, creating IPE opportunities for faculty and students at Wichita State. Brandy is an active member of Wichita Women for Good and Soroptimist, with the goal to empower women and girls. Brandy is a TeamSTEPPS master trainer. She received the DASIY Award for Extraordinary Nursing Faculty in 2019 at Wichita State University.
Brandy Jackson serves as the Director of Undergraduate Nursing Programs and Assistant Educator at Wichita State University and Co-Director of Access in Nursing. Brandy is a seasoned educator with over 15 years of experience. Before entering academia, Brandy served in Hospital-based leadership and Critical Care Staff nurse roles. Brandy is passionate about equity in nursing education with a focus on individuals with disabilities. Her current research interests include accommodations of nursing students with disabilities in clinical learning environments and breaking down barriers for historically unrepresented individuals to enter the nursing profession. Brandy is also actively engaged in Interprofessional Education development, creating IPE opportunities for faculty and students at Wichita State. Brandy is an active member of Wichita Women for Good and Soroptimist, with the goal to empower women and girls. Brandy is a TeamSTEPPS master trainer. She received the DASIY Award for Extraordinary Nursing Faculty in 2019 at Wichita State University.  Dr. Sabrina Ali Jamal-Eddine is an Arab-disabled queer woman of color with a PhD in Nursing and an interdisciplinary certificate in Disability Ethics from the University of Illinois Chicago (UIC). Dr. Jamal-Eddine’s doctoral research explored spoken word poetry as a form of critical narrative pedagogy to educate nursing students about disability, ableism, and disability justice. Dr. Jamal-Eddine now serves as a Postdoctoral Research Associate in UIC’s Department of Disability and Human Development and serves on the Board of Directors of the National Organization of Nurses with Disabilities (NOND). During her doctoral program, Sabrina served as a Summer Fellow at a residential National Endowment of the Humanities (NEH) Summer Institute at Arizona State University (2023), a summer fellow at Andrew W. Mellon’s National Humanities Without Walls program at University of Michigan (2022), a Summer Research Fellow at UC Berkeley’s Othering & Belonging Institute (2021), and an Illinois Leadership Education in Neurodevelopmental and related Disabilities (LEND) trainee (2019-2020).
Dr. Sabrina Ali Jamal-Eddine is an Arab-disabled queer woman of color with a PhD in Nursing and an interdisciplinary certificate in Disability Ethics from the University of Illinois Chicago (UIC). Dr. Jamal-Eddine’s doctoral research explored spoken word poetry as a form of critical narrative pedagogy to educate nursing students about disability, ableism, and disability justice. Dr. Jamal-Eddine now serves as a Postdoctoral Research Associate in UIC’s Department of Disability and Human Development and serves on the Board of Directors of the National Organization of Nurses with Disabilities (NOND). During her doctoral program, Sabrina served as a Summer Fellow at a residential National Endowment of the Humanities (NEH) Summer Institute at Arizona State University (2023), a summer fellow at Andrew W. Mellon’s National Humanities Without Walls program at University of Michigan (2022), a Summer Research Fellow at UC Berkeley’s Othering & Belonging Institute (2021), and an Illinois Leadership Education in Neurodevelopmental and related Disabilities (LEND) trainee (2019-2020). Vanessa Cameron works for Vanderbilt University Medical Center in Nursing Education & Professional Development. She is also attending George Washington University and progressing towards a PhD in Nursing with an emphasis on ableism in nursing. After becoming disabled in April 2021, Vanessa’s worldview and perspective changed, and a recognition of the ableism present within healthcare and within the culture of nursing was apparent. She has been working since that time to provide educational foundations for nurses about disability and ableism, provide support for fellow disabled nursing colleagues, and advocate for the disabled community within healthcare settings to reduce disparities.
Vanessa Cameron works for Vanderbilt University Medical Center in Nursing Education & Professional Development. She is also attending George Washington University and progressing towards a PhD in Nursing with an emphasis on ableism in nursing. After becoming disabled in April 2021, Vanessa’s worldview and perspective changed, and a recognition of the ableism present within healthcare and within the culture of nursing was apparent. She has been working since that time to provide educational foundations for nurses about disability and ableism, provide support for fellow disabled nursing colleagues, and advocate for the disabled community within healthcare settings to reduce disparities. Dr. Lucinda Canty is a certified nurse-midwife, Associate Professor of Nursing, and Director of the Seedworks Health Equity in Nursing Program at the University of Massachusetts Amherst. She earned a bachelor’s degree in nursing from Columbia University, a master’s degree from Yale University, specializing in nurse-midwifery, and a PhD from the University of Connecticut. Dr. Canty has provided reproductive health care for over 29 years. Her research interests include the prevention of maternal mortality and severe maternal morbidity, reducing racial and ethnic health disparities in reproductive health, promoting diversity in nursing, and eliminating racism in nursing and midwifery.
Dr. Lucinda Canty is a certified nurse-midwife, Associate Professor of Nursing, and Director of the Seedworks Health Equity in Nursing Program at the University of Massachusetts Amherst. She earned a bachelor’s degree in nursing from Columbia University, a master’s degree from Yale University, specializing in nurse-midwifery, and a PhD from the University of Connecticut. Dr. Canty has provided reproductive health care for over 29 years. Her research interests include the prevention of maternal mortality and severe maternal morbidity, reducing racial and ethnic health disparities in reproductive health, promoting diversity in nursing, and eliminating racism in nursing and midwifery. Dr. Lisa Meeks is a distinguished scholar and leader whose unwavering commitment to inclusivity and excellence has significantly influenced the landscape of health professions education and accessibility. She is the founder and executive director of the DocsWithDisabilities Initiative and holds appointments as an Associate Professor in the Departments of Learning Health Sciences and Family Medicine at the University of Michigan.
Dr. Lisa Meeks is a distinguished scholar and leader whose unwavering commitment to inclusivity and excellence has significantly influenced the landscape of health professions education and accessibility. She is the founder and executive director of the DocsWithDisabilities Initiative and holds appointments as an Associate Professor in the Departments of Learning Health Sciences and Family Medicine at the University of Michigan. Dr. Nikia Grayson, DNP, MSN, MPH, MA, CNM, FNP-C, FACNM (she/her) is a trailblazing force in reproductive justice, blending her expertise as a public health activist, anthropologist, and family nurse-midwife to champion the rights and health of underserved communities. Graduating with distinction from Howard University, Nikia holds a bachelor’s degree in communications and a master’s degree in public health. Her academic journey also led her to the University of Memphis, where she earned a master’s in medical anthropology, and the University of Tennessee, where she achieved both a master’s in nursing and a doctorate in nursing practice. Complementing her extensive education, she completed a post-master’s certificate in midwifery at Frontier Nursing University.
Dr. Nikia Grayson, DNP, MSN, MPH, MA, CNM, FNP-C, FACNM (she/her) is a trailblazing force in reproductive justice, blending her expertise as a public health activist, anthropologist, and family nurse-midwife to champion the rights and health of underserved communities. Graduating with distinction from Howard University, Nikia holds a bachelor’s degree in communications and a master’s degree in public health. Her academic journey also led her to the University of Memphis, where she earned a master’s in medical anthropology, and the University of Tennessee, where she achieved both a master’s in nursing and a doctorate in nursing practice. Complementing her extensive education, she completed a post-master’s certificate in midwifery at Frontier Nursing University.









 Dr. Tia Brown McNair is the Vice President in the Office of Diversity, Equity, and Student Success and Executive Director for the Truth, Racial Healing, and Transformation (TRHT) Campus Centers at the American Association of Colleges and Universities (AAC&U) in Washington, DC. She oversees both funded projects and AAC&U’s continuing programs on equity, inclusive excellence, high-impact practices, and student success. McNair directs AAC&U’s Summer Institutes on High-Impact Practices and Student Success, and TRHT Campus Centers and serves as the project director for several AAC&U initiatives, including the development of a TRHT-focused campus climate toolkit. She is the lead author of From Equity Talk to Equity Walk: Expanding Practitioner Knowledge for Racial Justice in Higher Education (January 2020) and Becoming a Student-Ready College: A New Culture of Leadership for Student Success (July 2016 and August 2022 Second edition).
Dr. Tia Brown McNair is the Vice President in the Office of Diversity, Equity, and Student Success and Executive Director for the Truth, Racial Healing, and Transformation (TRHT) Campus Centers at the American Association of Colleges and Universities (AAC&U) in Washington, DC. She oversees both funded projects and AAC&U’s continuing programs on equity, inclusive excellence, high-impact practices, and student success. McNair directs AAC&U’s Summer Institutes on High-Impact Practices and Student Success, and TRHT Campus Centers and serves as the project director for several AAC&U initiatives, including the development of a TRHT-focused campus climate toolkit. She is the lead author of From Equity Talk to Equity Walk: Expanding Practitioner Knowledge for Racial Justice in Higher Education (January 2020) and Becoming a Student-Ready College: A New Culture of Leadership for Student Success (July 2016 and August 2022 Second edition).