 At the heart of Frontier Nursing University is a talented and diverse community of students, alumni, faculty, staff, Couriers and preceptors. Spotlight blogs feature members of our FNU community who are focused on the mission of educating nurse-midwives and nurse practitioners to deliver quality healthcare to underserved and rural populations.
At the heart of Frontier Nursing University is a talented and diverse community of students, alumni, faculty, staff, Couriers and preceptors. Spotlight blogs feature members of our FNU community who are focused on the mission of educating nurse-midwives and nurse practitioners to deliver quality healthcare to underserved and rural populations.
It’s one thing to identify a problem. It’s quite another to find a solution. Yet that is what FNU Doctor of Nursing Practice (DNP) Alumni Kimberly Jones-Beatty, CNM, DNP, Class 37, is striving to do.
The problem has become increasingly well known, as the alarming numbers depicting the maternal mortality crisis in the United States persist. In 2018, there were 17 maternal deaths for every 100,000 live births in the U.S. — a ratio more than double that of most other high-income countries, and the U.S. has the highest maternal mortality rate among developed countries.^ The data is even more concerning for Black and American Indian/Alaska Native (AIAN) women, who have pregnancy-related mortality rates that are over three and two times higher, respectively, compared to the rate for white women.*
The data confirm the problem, but it does not offer a solution. Jones-Beatty, who works as a certified nurse-midwife within the OB/GYN department at Johns Hopkins University in Baltimore, Maryland, has been practicing midwifery for 12 years.
“I work in a dual clinical/research role through providing ambulatory obstetric care and overseeing clinical research in the Johns Hopkins Integrated Research Center for Fetal Medicine,” Jones-Beatty said. “As a clinical practitioner, I strive to provide evidence-based care. As a researcher, I see that we contribute to evidence-based care through translational research; by generating new knowledge or validating existing knowledge in both basic science and clinical research and applying it to clinical practice to improve patient care and outcomes. It’s the best of both worlds.”
Jones-Beatty put her research passion and skills to work in her DNP project, which focused on learning more about the maternal mortality crisis and its potential solutions.
“My DNP project focused on improving postpartum care,” she said. “Maternal morbidity and mortality are at an all-time high in the United States, and research shows that the majority of cases occur within the postpartum period. The American College of Obstetricians & Gynecologists (ACOG) has called for a paradigm shift in postpartum care by moving away from the single six-week visit and instead incorporating an ongoing postpartum process beginning in the antenatal period to impact adverse pregnancy outcomes and maternal morbidity and mortality rates. The aim of the project was to increase effective postpartum care through patient preparedness, early one-to-three-week patient follow-up, and comprehensive postpartum visits from 0% to 80% in eight weeks.”
To implement the project, Jones-Beatty followed ACOG’s recommendations in creating a postpartum planning tool. The tool included reviewing the importance of postpartum care and postpartum warning signs that warrant further evaluation. It also incorporated a population health registry for early one-to-three-week postpartum follow-up to ensure that postpartum patients were recovering from childbirth as expected and a comprehensive postpartum note template to help provide complete documentation of recommended postpartum visit components.
“The project aim was met at 88%,” Jones-Beatty said. “The planning tool effectively increased patients’ knowledge of postpartum warning signs. The registry was effective in obtaining postpartum right care scores, which translates into patients recovering from childbirth as expected. The note template was effective in guiding effective postpartum care office visits. Next steps will include reviewing the impact of the interventions on clinic-specific patient populations, overall maternal morbidity and mortality rates, and examining differences by race.”
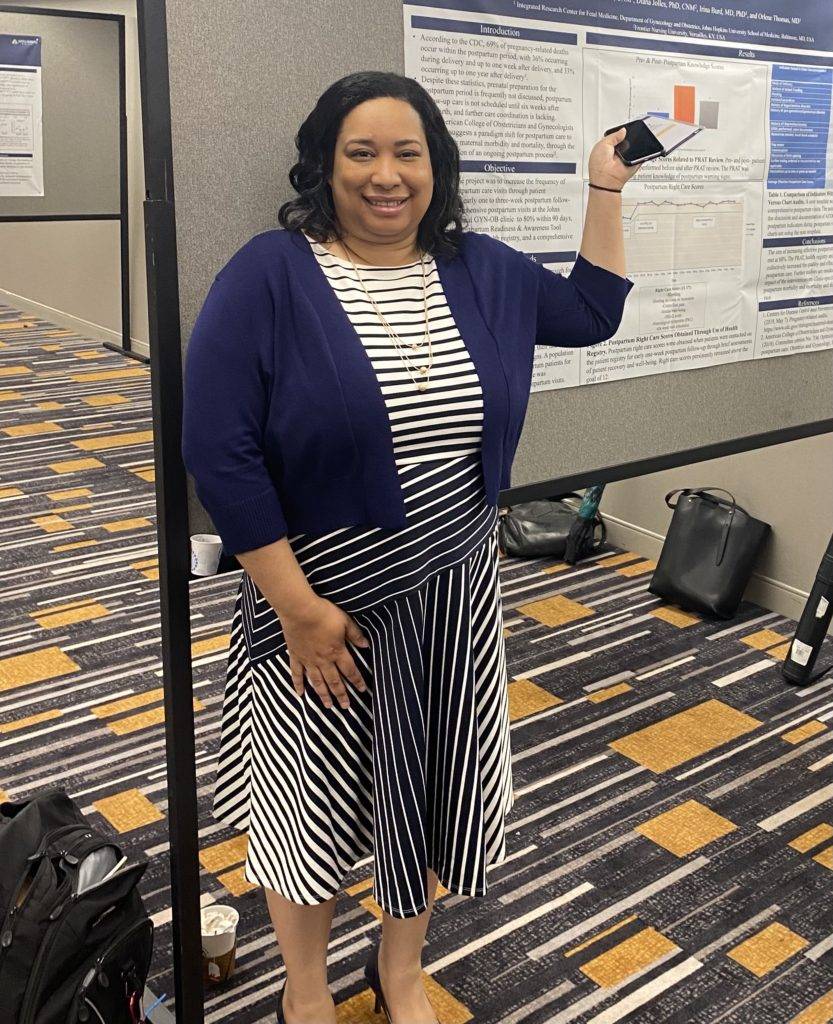 While more study and research are required to address maternal mortality, Jones-Beatty’s work was duly recognized for its significance. She recently presented her project as a poster presentation at the Society for Reproductive Investigation’s Annual Meeting in Boston, Massachusetts.
While more study and research are required to address maternal mortality, Jones-Beatty’s work was duly recognized for its significance. She recently presented her project as a poster presentation at the Society for Reproductive Investigation’s Annual Meeting in Boston, Massachusetts.
“Attending the meeting was a great experience, with networking opportunities and the chance to hear about new practice perspectives, guidelines, and other original research within reproductive health,” she said.
Jones-Beatty’s love for research and information paired well with Frontier’s emphasis on data-driven analysis and decision-making.
“I decided to pursue a doctorate in nursing practice at Frontier due to its strong reputation, online format, and faculty expertise,” she said. “FNU’s DNP curriculum provides instruction on leading quality improvement in the clinical setting, as well as exposure to evidence-based practice, health policy and advocacy, and system/ organizational leadership. Collectively, I feel prepared to impact any healthcare setting I choose to work in through a deep understanding of the education and skills that exemplify nurse leaders who are ready to change the landscape of the current healthcare environment.”
Jones-Beatty is well-prepared to continue to excel as both a researcher and a clinician. Both roles hold equal value to her as she seeks to positively impact her current and future patients and colleagues.
“I plan to continue working both clinically and in research, contributing to evidence-based practice, improving obstetric healthcare, and decreasing adverse pregnancy and neonatal outcomes,” she said.
FNU is proud of Jones-Beatty for her dedication to research and midwifery. She is a shining example of bringing FNU’s Culture of Caring to her community.
Interested in reading more stories about our alumni? Visit the FNU Alumni stories page.
^Roosa Tikkanen et al., Maternal Mortality and Maternity Care in the United States Compared to 10 Other Developed Countries (Commonwealth Fund, Nov. 2020). https://doi.org/10.26099/411v-9255
*Artiga, S., Pham, O., Orgera, K., Ranji, U. (2020). Racial Disparities in Maternal and Infant
Health: An Overview. Issue Brief. Kaiser Family Foundation, November 10, 2020


 By: Dr. Susan Stone, Frontier Nursing University President
By: Dr. Susan Stone, Frontier Nursing University President With the above statistics in mind, it is more important than ever to develop and begin working toward attainable solutions.
With the above statistics in mind, it is more important than ever to develop and begin working toward attainable solutions. 

 Dr. Susan Stone, DNSc, CNM, FACNM, FAAN, certified nurse-midwife, President of Frontier Nursing University (FNU) and President of the American College of Nurse-Midwives (ACNM), recently sat down with Andrew Bennie of Springer Publishing Group to continue the ongoing conversation about how to end maternal mortality. Dr. Stone has been working in the field of reproductive health care for women for over 30 years, and is an advocate for women seeking an emotional and physically satisfying childbirth.
Dr. Susan Stone, DNSc, CNM, FACNM, FAAN, certified nurse-midwife, President of Frontier Nursing University (FNU) and President of the American College of Nurse-Midwives (ACNM), recently sat down with Andrew Bennie of Springer Publishing Group to continue the ongoing conversation about how to end maternal mortality. Dr. Stone has been working in the field of reproductive health care for women for over 30 years, and is an advocate for women seeking an emotional and physically satisfying childbirth.


















 Carrie Belin is an experienced board-certified Family Nurse Practitioner and a graduate of the Johns Hopkins DNP program, Johns Hopkins Bloomberg School of Public Health, Georgetown University School of Nursing, and Johns Hopkins School of Nursing. She has also completed fellowships at Georgetown and the University of California Irvine.
Carrie Belin is an experienced board-certified Family Nurse Practitioner and a graduate of the Johns Hopkins DNP program, Johns Hopkins Bloomberg School of Public Health, Georgetown University School of Nursing, and Johns Hopkins School of Nursing. She has also completed fellowships at Georgetown and the University of California Irvine. Angie has been a full-scope midwife since 2009. She has experience in various birth settings including home, hospital, and birth centers. She is committed to integrating the midwifery model of care in the US. She completed her master’s degree in nurse-midwifery at Frontier Nursing University (FNU) and her Doctorate at Johns Hopkins University. She currently serves as the midwifery clinical faculty at FNU. Angie is motivated by the desire to improve the quality of healthcare and has led quality improvement projects on skin-to-skin implementation, labor induction, and improving transfer of care practices between hospital and community midwives. In 2017, she created a short film on skin-to-skin called
Angie has been a full-scope midwife since 2009. She has experience in various birth settings including home, hospital, and birth centers. She is committed to integrating the midwifery model of care in the US. She completed her master’s degree in nurse-midwifery at Frontier Nursing University (FNU) and her Doctorate at Johns Hopkins University. She currently serves as the midwifery clinical faculty at FNU. Angie is motivated by the desire to improve the quality of healthcare and has led quality improvement projects on skin-to-skin implementation, labor induction, and improving transfer of care practices between hospital and community midwives. In 2017, she created a short film on skin-to-skin called 










 Justin C. Daily, BSN, RN, has ten years of experience in nursing. At the start of his nursing career, Justin worked as a floor nurse on the oncology floor at St. Francis. He then spent two years as the Director of Nursing in a small rural Kansas hospital before returning to St. Francis and the oncology unit. He has been in his current position as the Chemo Nurse Educator for the past four years. He earned an Associate in Nurse from Hutchinson Community College and a Bachelor of Science in Nursing from Bethel College.
Justin C. Daily, BSN, RN, has ten years of experience in nursing. At the start of his nursing career, Justin worked as a floor nurse on the oncology floor at St. Francis. He then spent two years as the Director of Nursing in a small rural Kansas hospital before returning to St. Francis and the oncology unit. He has been in his current position as the Chemo Nurse Educator for the past four years. He earned an Associate in Nurse from Hutchinson Community College and a Bachelor of Science in Nursing from Bethel College. Brandy Jackson serves as the Director of Undergraduate Nursing Programs and Assistant Educator at Wichita State University and Co-Director of Access in Nursing. Brandy is a seasoned educator with over 15 years of experience. Before entering academia, Brandy served in Hospital-based leadership and Critical Care Staff nurse roles. Brandy is passionate about equity in nursing education with a focus on individuals with disabilities. Her current research interests include accommodations of nursing students with disabilities in clinical learning environments and breaking down barriers for historically unrepresented individuals to enter the nursing profession. Brandy is also actively engaged in Interprofessional Education development, creating IPE opportunities for faculty and students at Wichita State. Brandy is an active member of Wichita Women for Good and Soroptimist, with the goal to empower women and girls. Brandy is a TeamSTEPPS master trainer. She received the DASIY Award for Extraordinary Nursing Faculty in 2019 at Wichita State University.
Brandy Jackson serves as the Director of Undergraduate Nursing Programs and Assistant Educator at Wichita State University and Co-Director of Access in Nursing. Brandy is a seasoned educator with over 15 years of experience. Before entering academia, Brandy served in Hospital-based leadership and Critical Care Staff nurse roles. Brandy is passionate about equity in nursing education with a focus on individuals with disabilities. Her current research interests include accommodations of nursing students with disabilities in clinical learning environments and breaking down barriers for historically unrepresented individuals to enter the nursing profession. Brandy is also actively engaged in Interprofessional Education development, creating IPE opportunities for faculty and students at Wichita State. Brandy is an active member of Wichita Women for Good and Soroptimist, with the goal to empower women and girls. Brandy is a TeamSTEPPS master trainer. She received the DASIY Award for Extraordinary Nursing Faculty in 2019 at Wichita State University.  Dr. Sabrina Ali Jamal-Eddine is an Arab-disabled queer woman of color with a PhD in Nursing and an interdisciplinary certificate in Disability Ethics from the University of Illinois Chicago (UIC). Dr. Jamal-Eddine’s doctoral research explored spoken word poetry as a form of critical narrative pedagogy to educate nursing students about disability, ableism, and disability justice. Dr. Jamal-Eddine now serves as a Postdoctoral Research Associate in UIC’s Department of Disability and Human Development and serves on the Board of Directors of the National Organization of Nurses with Disabilities (NOND). During her doctoral program, Sabrina served as a Summer Fellow at a residential National Endowment of the Humanities (NEH) Summer Institute at Arizona State University (2023), a summer fellow at Andrew W. Mellon’s National Humanities Without Walls program at University of Michigan (2022), a Summer Research Fellow at UC Berkeley’s Othering & Belonging Institute (2021), and an Illinois Leadership Education in Neurodevelopmental and related Disabilities (LEND) trainee (2019-2020).
Dr. Sabrina Ali Jamal-Eddine is an Arab-disabled queer woman of color with a PhD in Nursing and an interdisciplinary certificate in Disability Ethics from the University of Illinois Chicago (UIC). Dr. Jamal-Eddine’s doctoral research explored spoken word poetry as a form of critical narrative pedagogy to educate nursing students about disability, ableism, and disability justice. Dr. Jamal-Eddine now serves as a Postdoctoral Research Associate in UIC’s Department of Disability and Human Development and serves on the Board of Directors of the National Organization of Nurses with Disabilities (NOND). During her doctoral program, Sabrina served as a Summer Fellow at a residential National Endowment of the Humanities (NEH) Summer Institute at Arizona State University (2023), a summer fellow at Andrew W. Mellon’s National Humanities Without Walls program at University of Michigan (2022), a Summer Research Fellow at UC Berkeley’s Othering & Belonging Institute (2021), and an Illinois Leadership Education in Neurodevelopmental and related Disabilities (LEND) trainee (2019-2020). Vanessa Cameron works for Vanderbilt University Medical Center in Nursing Education & Professional Development. She is also attending George Washington University and progressing towards a PhD in Nursing with an emphasis on ableism in nursing. After becoming disabled in April 2021, Vanessa’s worldview and perspective changed, and a recognition of the ableism present within healthcare and within the culture of nursing was apparent. She has been working since that time to provide educational foundations for nurses about disability and ableism, provide support for fellow disabled nursing colleagues, and advocate for the disabled community within healthcare settings to reduce disparities.
Vanessa Cameron works for Vanderbilt University Medical Center in Nursing Education & Professional Development. She is also attending George Washington University and progressing towards a PhD in Nursing with an emphasis on ableism in nursing. After becoming disabled in April 2021, Vanessa’s worldview and perspective changed, and a recognition of the ableism present within healthcare and within the culture of nursing was apparent. She has been working since that time to provide educational foundations for nurses about disability and ableism, provide support for fellow disabled nursing colleagues, and advocate for the disabled community within healthcare settings to reduce disparities. Dr. Lucinda Canty is a certified nurse-midwife, Associate Professor of Nursing, and Director of the Seedworks Health Equity in Nursing Program at the University of Massachusetts Amherst. She earned a bachelor’s degree in nursing from Columbia University, a master’s degree from Yale University, specializing in nurse-midwifery, and a PhD from the University of Connecticut. Dr. Canty has provided reproductive health care for over 29 years. Her research interests include the prevention of maternal mortality and severe maternal morbidity, reducing racial and ethnic health disparities in reproductive health, promoting diversity in nursing, and eliminating racism in nursing and midwifery.
Dr. Lucinda Canty is a certified nurse-midwife, Associate Professor of Nursing, and Director of the Seedworks Health Equity in Nursing Program at the University of Massachusetts Amherst. She earned a bachelor’s degree in nursing from Columbia University, a master’s degree from Yale University, specializing in nurse-midwifery, and a PhD from the University of Connecticut. Dr. Canty has provided reproductive health care for over 29 years. Her research interests include the prevention of maternal mortality and severe maternal morbidity, reducing racial and ethnic health disparities in reproductive health, promoting diversity in nursing, and eliminating racism in nursing and midwifery. Dr. Lisa Meeks is a distinguished scholar and leader whose unwavering commitment to inclusivity and excellence has significantly influenced the landscape of health professions education and accessibility. She is the founder and executive director of the DocsWithDisabilities Initiative and holds appointments as an Associate Professor in the Departments of Learning Health Sciences and Family Medicine at the University of Michigan.
Dr. Lisa Meeks is a distinguished scholar and leader whose unwavering commitment to inclusivity and excellence has significantly influenced the landscape of health professions education and accessibility. She is the founder and executive director of the DocsWithDisabilities Initiative and holds appointments as an Associate Professor in the Departments of Learning Health Sciences and Family Medicine at the University of Michigan. Dr. Nikia Grayson, DNP, MSN, MPH, MA, CNM, FNP-C, FACNM (she/her) is a trailblazing force in reproductive justice, blending her expertise as a public health activist, anthropologist, and family nurse-midwife to champion the rights and health of underserved communities. Graduating with distinction from Howard University, Nikia holds a bachelor’s degree in communications and a master’s degree in public health. Her academic journey also led her to the University of Memphis, where she earned a master’s in medical anthropology, and the University of Tennessee, where she achieved both a master’s in nursing and a doctorate in nursing practice. Complementing her extensive education, she completed a post-master’s certificate in midwifery at Frontier Nursing University.
Dr. Nikia Grayson, DNP, MSN, MPH, MA, CNM, FNP-C, FACNM (she/her) is a trailblazing force in reproductive justice, blending her expertise as a public health activist, anthropologist, and family nurse-midwife to champion the rights and health of underserved communities. Graduating with distinction from Howard University, Nikia holds a bachelor’s degree in communications and a master’s degree in public health. Her academic journey also led her to the University of Memphis, where she earned a master’s in medical anthropology, and the University of Tennessee, where she achieved both a master’s in nursing and a doctorate in nursing practice. Complementing her extensive education, she completed a post-master’s certificate in midwifery at Frontier Nursing University.









 Dr. Tia Brown McNair is the Vice President in the Office of Diversity, Equity, and Student Success and Executive Director for the Truth, Racial Healing, and Transformation (TRHT) Campus Centers at the American Association of Colleges and Universities (AAC&U) in Washington, DC. She oversees both funded projects and AAC&U’s continuing programs on equity, inclusive excellence, high-impact practices, and student success. McNair directs AAC&U’s Summer Institutes on High-Impact Practices and Student Success, and TRHT Campus Centers and serves as the project director for several AAC&U initiatives, including the development of a TRHT-focused campus climate toolkit. She is the lead author of From Equity Talk to Equity Walk: Expanding Practitioner Knowledge for Racial Justice in Higher Education (January 2020) and Becoming a Student-Ready College: A New Culture of Leadership for Student Success (July 2016 and August 2022 Second edition).
Dr. Tia Brown McNair is the Vice President in the Office of Diversity, Equity, and Student Success and Executive Director for the Truth, Racial Healing, and Transformation (TRHT) Campus Centers at the American Association of Colleges and Universities (AAC&U) in Washington, DC. She oversees both funded projects and AAC&U’s continuing programs on equity, inclusive excellence, high-impact practices, and student success. McNair directs AAC&U’s Summer Institutes on High-Impact Practices and Student Success, and TRHT Campus Centers and serves as the project director for several AAC&U initiatives, including the development of a TRHT-focused campus climate toolkit. She is the lead author of From Equity Talk to Equity Walk: Expanding Practitioner Knowledge for Racial Justice in Higher Education (January 2020) and Becoming a Student-Ready College: A New Culture of Leadership for Student Success (July 2016 and August 2022 Second edition).