 Even as a child, FNU alumni Holly Howell, MSN, CNM, knew she wanted to be a nurse. It was a not-so-subtle nudge that pushed her in the right direction.
Even as a child, FNU alumni Holly Howell, MSN, CNM, knew she wanted to be a nurse. It was a not-so-subtle nudge that pushed her in the right direction.
“At a very young age, I have a very vivid memory of my aunt, heavily pregnant, asking me to feel her belly, and the baby made a really large movement,” Howell said. “In my head, it’s still the largest movement I’ve ever felt from a baby. I was fascinated and intrigued by it. From then on, I knew that I wanted to work in the maternal-child field. I wanted to deliver babies. It was my end goal. I’m really proud of myself that I made it, and I’m doing it.”
Howell grew up in Nevada and earned a Bachelor of Science in Nursing from Nevada State College, becoming the first woman in her family to graduate from college. With her focus on attending births and caring for pregnant women, she chose Frontier Nursing University to guide her to her goal of becoming a Certified Nurse-Midwife. During her time at FNU, she was awarded the Jesse Smith Noyes Scholarship.
“Receiving the scholarship definitely helped me to complete the program at Frontier and also relieved some of the burdens of student loan debt,” she said. “Frontier prepared me really well for midwifery care and caring for patients. It has also given me a great network of midwifery friends and partners that I can lean on during stressful times and reach out to for questions or similar experiences. Those deep bonds were created during on-campus sessions and study groups as we went through the program together, leaning on each other during stressful times. Since then, we have been able to stay in contact via social media really well.”
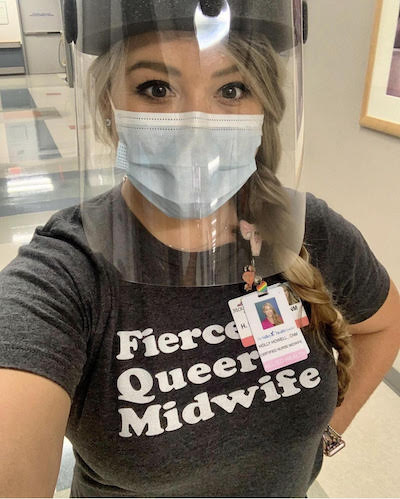 Today, Howell works as a nurse-midwife at two different locations in Las Vegas, both of which are part of the Women’s Health Associates of Southern Nevada. Her usual routine includes morning rounds at the hospital before arriving at the clinic between 8:45 and 9:00 a.m. The clinic includes three collaborating physician partners and two collaborating midwifery partners in addition to Howell. She sees between 25 and 35 patients per day.
Today, Howell works as a nurse-midwife at two different locations in Las Vegas, both of which are part of the Women’s Health Associates of Southern Nevada. Her usual routine includes morning rounds at the hospital before arriving at the clinic between 8:45 and 9:00 a.m. The clinic includes three collaborating physician partners and two collaborating midwifery partners in addition to Howell. She sees between 25 and 35 patients per day.
“They are primarily pregnant and OB patients, but I do also do birth control consults, menopausal care, annual exams, and IUD insertions,” she said. “We’re a very busy OB practice, and I see primarily pregnant people and postpartum visits. I also deliver quite a few babies every month, so I’m in and out of the hospital all the time. Yesterday (March 22, 2022), I actually set a record for myself and delivered five of my own babies in a 24- hour period. I didn’t sleep much.”
It was yet another taxing day in what has been a taxing two years during the COVID-19 pandemic. Howell has relied on her training and knowledge to try to be a steadying and calming influence for her patients.
“The pandemic has been really scary and taxing for a lot of people, especially for pregnant people,” Howell said. “They have been very anxious during the pandemic and have needed a lot of support, education, and reassurance.”
With several of her patients contracting COVID, Howell saw first-hand the additional risks that pregnant women faced.
 “During labor and birth, I pride myself on making sure that I’m practicing in an evidence-based way and that I am giving family-centered and patient-centered care.”
“During labor and birth, I pride myself on making sure that I’m practicing in an evidence-based way and that I am giving family-centered and patient-centered care.”
– Holly Howell, MSN, CNM, FNU Alumni
“We saw how it could affect pregnant people and how they have an increased risk of getting sicker than the normal population,” Howell said. “I’ve been doing a lot of counseling and education that I was doing before, but it’s a little bit more sensitive because they know that they are at a higher risk for getting more severe symptoms than a non-pregnant person.”
Howell also counseled patients about the vaccines. She helped them through their understandable fear and anxiety by “staying up to date with all of the current recommendations so I could give my patients good evidence-based answers to the questions.”
 As if the pandemic was not difficult enough to cope with, Howell and her wife Dana faced their own personal tragedy late last year.
As if the pandemic was not difficult enough to cope with, Howell and her wife Dana faced their own personal tragedy late last year.
“I gave birth to my son Huck Wilder at 20 weeks gestation,” Howell said. “It’s a very scary and traumatic way to be on the other side and be the patient. I had really amazing nurses and a certified nurse-midwife that took great care of me. But I just love him and miss him every day. I’m grateful that I had him and that he was here, and I am grateful for the opportunity to be a patient and to be on the other side of women’s health. I think going through this experience will make me a better, more empathetic provider. I’m sad that I had to experience that, but really am grateful for the time that I did have with him.”
Though pained, Howell speaks openly about her experience and the immeasurable impact Huck has had on her.
“He has been an inspiration for me to take really good care of pregnant people and also try to decrease the traumatic birth experience that people and families have during labor and birth,” she said. “I also had a really severe postpartum hemorrhage and do have some PTSD and trauma from my birth with no fault to my providers at all, just to the situation. My experience losing Huck has definitely given me insight and motivated me to provide the best care I can for birthing people and families.”
Perhaps that is why Howell is much more than a provider. She states in her own profile on the Women’s Health Associates of Southern Nevada that she “is an advocate empowering women, natural childbirth, breastfeeding, women’s reproductive rights, and health equality for the LGBTQIA+ community.” One example of how she advocates for her patients is she has stopped using stirrups during pelvic exams and births unless the patient requests them. She finds that this gives the patient more autonomy over their own body and better freedom of movement.
 “I pride myself on practicing in a trauma-informed way,” Howell said. “I always ask for consent and permission before I do any kind of pelvic or invasive exam. During labor and birth, I pride myself on making sure that I’m practicing in an evidence-based way and that I am giving family-centered and patient-centered care. I give patients options, and we have in-depth discussions before any interventions are completed, making sure that they are well educated about their bodies and their different options during labor and childbirth.”
“I pride myself on practicing in a trauma-informed way,” Howell said. “I always ask for consent and permission before I do any kind of pelvic or invasive exam. During labor and birth, I pride myself on making sure that I’m practicing in an evidence-based way and that I am giving family-centered and patient-centered care. I give patients options, and we have in-depth discussions before any interventions are completed, making sure that they are well educated about their bodies and their different options during labor and childbirth.”
In addition to educating and informing her patients, Howell wants to make sure her patients feel accepted and welcomed into a clinic that is safe and inclusive.
“I am a proud gay woman and advertise that on my website,” Howell said. “Hopefully, LGBTQIA+ people can come and see me and find a safe environment where they can be free to be themselves and be more comfortable with invasive exams and care.”
Howell dreams of one day opening her own birth center, but for now, she is happy right where she is at, living out her childhood dreams every day, to the significant benefit of her community.
“We provide really great service to a lot of women and give them a happy medium between home birth or birth center care,” she said. “I’m really happy being a resource for the women who are not eligible for home birth or birth center care because I can still give them that low intervention, calm environment in the hospital setting. I am very happy with where I am at.”
To read more spotlight stories on the important work our alumni are doing, please visit this page.




















 Carrie Belin is an experienced board-certified Family Nurse Practitioner and a graduate of the Johns Hopkins DNP program, Johns Hopkins Bloomberg School of Public Health, Georgetown University School of Nursing, and Johns Hopkins School of Nursing. She has also completed fellowships at Georgetown and the University of California Irvine.
Carrie Belin is an experienced board-certified Family Nurse Practitioner and a graduate of the Johns Hopkins DNP program, Johns Hopkins Bloomberg School of Public Health, Georgetown University School of Nursing, and Johns Hopkins School of Nursing. She has also completed fellowships at Georgetown and the University of California Irvine. Angie has been a full-scope midwife since 2009. She has experience in various birth settings including home, hospital, and birth centers. She is committed to integrating the midwifery model of care in the US. She completed her master’s degree in nurse-midwifery at Frontier Nursing University (FNU) and her Doctorate at Johns Hopkins University. She currently serves as the midwifery clinical faculty at FNU. Angie is motivated by the desire to improve the quality of healthcare and has led quality improvement projects on skin-to-skin implementation, labor induction, and improving transfer of care practices between hospital and community midwives. In 2017, she created a short film on skin-to-skin called
Angie has been a full-scope midwife since 2009. She has experience in various birth settings including home, hospital, and birth centers. She is committed to integrating the midwifery model of care in the US. She completed her master’s degree in nurse-midwifery at Frontier Nursing University (FNU) and her Doctorate at Johns Hopkins University. She currently serves as the midwifery clinical faculty at FNU. Angie is motivated by the desire to improve the quality of healthcare and has led quality improvement projects on skin-to-skin implementation, labor induction, and improving transfer of care practices between hospital and community midwives. In 2017, she created a short film on skin-to-skin called 










 Justin C. Daily, BSN, RN, has ten years of experience in nursing. At the start of his nursing career, Justin worked as a floor nurse on the oncology floor at St. Francis. He then spent two years as the Director of Nursing in a small rural Kansas hospital before returning to St. Francis and the oncology unit. He has been in his current position as the Chemo Nurse Educator for the past four years. He earned an Associate in Nurse from Hutchinson Community College and a Bachelor of Science in Nursing from Bethel College.
Justin C. Daily, BSN, RN, has ten years of experience in nursing. At the start of his nursing career, Justin worked as a floor nurse on the oncology floor at St. Francis. He then spent two years as the Director of Nursing in a small rural Kansas hospital before returning to St. Francis and the oncology unit. He has been in his current position as the Chemo Nurse Educator for the past four years. He earned an Associate in Nurse from Hutchinson Community College and a Bachelor of Science in Nursing from Bethel College. Brandy Jackson serves as the Director of Undergraduate Nursing Programs and Assistant Educator at Wichita State University and Co-Director of Access in Nursing. Brandy is a seasoned educator with over 15 years of experience. Before entering academia, Brandy served in Hospital-based leadership and Critical Care Staff nurse roles. Brandy is passionate about equity in nursing education with a focus on individuals with disabilities. Her current research interests include accommodations of nursing students with disabilities in clinical learning environments and breaking down barriers for historically unrepresented individuals to enter the nursing profession. Brandy is also actively engaged in Interprofessional Education development, creating IPE opportunities for faculty and students at Wichita State. Brandy is an active member of Wichita Women for Good and Soroptimist, with the goal to empower women and girls. Brandy is a TeamSTEPPS master trainer. She received the DASIY Award for Extraordinary Nursing Faculty in 2019 at Wichita State University.
Brandy Jackson serves as the Director of Undergraduate Nursing Programs and Assistant Educator at Wichita State University and Co-Director of Access in Nursing. Brandy is a seasoned educator with over 15 years of experience. Before entering academia, Brandy served in Hospital-based leadership and Critical Care Staff nurse roles. Brandy is passionate about equity in nursing education with a focus on individuals with disabilities. Her current research interests include accommodations of nursing students with disabilities in clinical learning environments and breaking down barriers for historically unrepresented individuals to enter the nursing profession. Brandy is also actively engaged in Interprofessional Education development, creating IPE opportunities for faculty and students at Wichita State. Brandy is an active member of Wichita Women for Good and Soroptimist, with the goal to empower women and girls. Brandy is a TeamSTEPPS master trainer. She received the DASIY Award for Extraordinary Nursing Faculty in 2019 at Wichita State University.  Dr. Sabrina Ali Jamal-Eddine is an Arab-disabled queer woman of color with a PhD in Nursing and an interdisciplinary certificate in Disability Ethics from the University of Illinois Chicago (UIC). Dr. Jamal-Eddine’s doctoral research explored spoken word poetry as a form of critical narrative pedagogy to educate nursing students about disability, ableism, and disability justice. Dr. Jamal-Eddine now serves as a Postdoctoral Research Associate in UIC’s Department of Disability and Human Development and serves on the Board of Directors of the National Organization of Nurses with Disabilities (NOND). During her doctoral program, Sabrina served as a Summer Fellow at a residential National Endowment of the Humanities (NEH) Summer Institute at Arizona State University (2023), a summer fellow at Andrew W. Mellon’s National Humanities Without Walls program at University of Michigan (2022), a Summer Research Fellow at UC Berkeley’s Othering & Belonging Institute (2021), and an Illinois Leadership Education in Neurodevelopmental and related Disabilities (LEND) trainee (2019-2020).
Dr. Sabrina Ali Jamal-Eddine is an Arab-disabled queer woman of color with a PhD in Nursing and an interdisciplinary certificate in Disability Ethics from the University of Illinois Chicago (UIC). Dr. Jamal-Eddine’s doctoral research explored spoken word poetry as a form of critical narrative pedagogy to educate nursing students about disability, ableism, and disability justice. Dr. Jamal-Eddine now serves as a Postdoctoral Research Associate in UIC’s Department of Disability and Human Development and serves on the Board of Directors of the National Organization of Nurses with Disabilities (NOND). During her doctoral program, Sabrina served as a Summer Fellow at a residential National Endowment of the Humanities (NEH) Summer Institute at Arizona State University (2023), a summer fellow at Andrew W. Mellon’s National Humanities Without Walls program at University of Michigan (2022), a Summer Research Fellow at UC Berkeley’s Othering & Belonging Institute (2021), and an Illinois Leadership Education in Neurodevelopmental and related Disabilities (LEND) trainee (2019-2020). Vanessa Cameron works for Vanderbilt University Medical Center in Nursing Education & Professional Development. She is also attending George Washington University and progressing towards a PhD in Nursing with an emphasis on ableism in nursing. After becoming disabled in April 2021, Vanessa’s worldview and perspective changed, and a recognition of the ableism present within healthcare and within the culture of nursing was apparent. She has been working since that time to provide educational foundations for nurses about disability and ableism, provide support for fellow disabled nursing colleagues, and advocate for the disabled community within healthcare settings to reduce disparities.
Vanessa Cameron works for Vanderbilt University Medical Center in Nursing Education & Professional Development. She is also attending George Washington University and progressing towards a PhD in Nursing with an emphasis on ableism in nursing. After becoming disabled in April 2021, Vanessa’s worldview and perspective changed, and a recognition of the ableism present within healthcare and within the culture of nursing was apparent. She has been working since that time to provide educational foundations for nurses about disability and ableism, provide support for fellow disabled nursing colleagues, and advocate for the disabled community within healthcare settings to reduce disparities. Dr. Lucinda Canty is a certified nurse-midwife, Associate Professor of Nursing, and Director of the Seedworks Health Equity in Nursing Program at the University of Massachusetts Amherst. She earned a bachelor’s degree in nursing from Columbia University, a master’s degree from Yale University, specializing in nurse-midwifery, and a PhD from the University of Connecticut. Dr. Canty has provided reproductive health care for over 29 years. Her research interests include the prevention of maternal mortality and severe maternal morbidity, reducing racial and ethnic health disparities in reproductive health, promoting diversity in nursing, and eliminating racism in nursing and midwifery.
Dr. Lucinda Canty is a certified nurse-midwife, Associate Professor of Nursing, and Director of the Seedworks Health Equity in Nursing Program at the University of Massachusetts Amherst. She earned a bachelor’s degree in nursing from Columbia University, a master’s degree from Yale University, specializing in nurse-midwifery, and a PhD from the University of Connecticut. Dr. Canty has provided reproductive health care for over 29 years. Her research interests include the prevention of maternal mortality and severe maternal morbidity, reducing racial and ethnic health disparities in reproductive health, promoting diversity in nursing, and eliminating racism in nursing and midwifery. Dr. Lisa Meeks is a distinguished scholar and leader whose unwavering commitment to inclusivity and excellence has significantly influenced the landscape of health professions education and accessibility. She is the founder and executive director of the DocsWithDisabilities Initiative and holds appointments as an Associate Professor in the Departments of Learning Health Sciences and Family Medicine at the University of Michigan.
Dr. Lisa Meeks is a distinguished scholar and leader whose unwavering commitment to inclusivity and excellence has significantly influenced the landscape of health professions education and accessibility. She is the founder and executive director of the DocsWithDisabilities Initiative and holds appointments as an Associate Professor in the Departments of Learning Health Sciences and Family Medicine at the University of Michigan. Dr. Nikia Grayson, DNP, MSN, MPH, MA, CNM, FNP-C, FACNM (she/her) is a trailblazing force in reproductive justice, blending her expertise as a public health activist, anthropologist, and family nurse-midwife to champion the rights and health of underserved communities. Graduating with distinction from Howard University, Nikia holds a bachelor’s degree in communications and a master’s degree in public health. Her academic journey also led her to the University of Memphis, where she earned a master’s in medical anthropology, and the University of Tennessee, where she achieved both a master’s in nursing and a doctorate in nursing practice. Complementing her extensive education, she completed a post-master’s certificate in midwifery at Frontier Nursing University.
Dr. Nikia Grayson, DNP, MSN, MPH, MA, CNM, FNP-C, FACNM (she/her) is a trailblazing force in reproductive justice, blending her expertise as a public health activist, anthropologist, and family nurse-midwife to champion the rights and health of underserved communities. Graduating with distinction from Howard University, Nikia holds a bachelor’s degree in communications and a master’s degree in public health. Her academic journey also led her to the University of Memphis, where she earned a master’s in medical anthropology, and the University of Tennessee, where she achieved both a master’s in nursing and a doctorate in nursing practice. Complementing her extensive education, she completed a post-master’s certificate in midwifery at Frontier Nursing University.









 Dr. Tia Brown McNair is the Vice President in the Office of Diversity, Equity, and Student Success and Executive Director for the Truth, Racial Healing, and Transformation (TRHT) Campus Centers at the American Association of Colleges and Universities (AAC&U) in Washington, DC. She oversees both funded projects and AAC&U’s continuing programs on equity, inclusive excellence, high-impact practices, and student success. McNair directs AAC&U’s Summer Institutes on High-Impact Practices and Student Success, and TRHT Campus Centers and serves as the project director for several AAC&U initiatives, including the development of a TRHT-focused campus climate toolkit. She is the lead author of From Equity Talk to Equity Walk: Expanding Practitioner Knowledge for Racial Justice in Higher Education (January 2020) and Becoming a Student-Ready College: A New Culture of Leadership for Student Success (July 2016 and August 2022 Second edition).
Dr. Tia Brown McNair is the Vice President in the Office of Diversity, Equity, and Student Success and Executive Director for the Truth, Racial Healing, and Transformation (TRHT) Campus Centers at the American Association of Colleges and Universities (AAC&U) in Washington, DC. She oversees both funded projects and AAC&U’s continuing programs on equity, inclusive excellence, high-impact practices, and student success. McNair directs AAC&U’s Summer Institutes on High-Impact Practices and Student Success, and TRHT Campus Centers and serves as the project director for several AAC&U initiatives, including the development of a TRHT-focused campus climate toolkit. She is the lead author of From Equity Talk to Equity Walk: Expanding Practitioner Knowledge for Racial Justice in Higher Education (January 2020) and Becoming a Student-Ready College: A New Culture of Leadership for Student Success (July 2016 and August 2022 Second edition).